Surgical Technique Steps
Patient Evaluation:
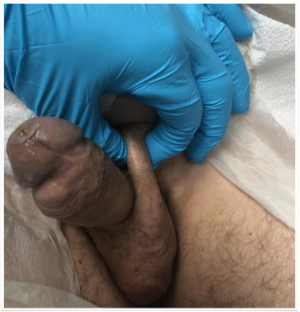
After a, thorough history and physical exam, we perform a penile Doppler to document irreversible, organic erectile dysfunction. This test is also a trial of injection therapy. We use the Doppler to give the patient a cause for their ED, in addition to showing them they are able to get erections again. The Doppler helps in identifying penile plaques or curvatures. Be careful with the patient that doesn’t get a full erection with the injections as they might still have occult penile curvatures. A full set of labs helps weed out poorly compliant diabetics or identify patients with hypogonadism. Do not deny patients with Low T an implant, as low T treatment does not cure ED in a patient that needs an implant.
All patients that have had a Radical Prostatectomy need a cystoscopy to make sure they don’t have bladder neck contractures. It is our custom to get urine cultures on all implant patients. Proper medical and cardiac clearances should be obtained as routine for the surgical procedure.
Patient cancellations:
There are several reasons patients cancel surgeries, the most common is external family factors and misconceptions. Patients families do not conceder ED as a significant illness and think men want implants so they can fool around with many women. Although true in some cases, most men want to be able to be restored to their natural state, to being a man again. Whether they choose to have sex is a totally different issue. Implant cure ED, they cure the depression that comes with ED and can be instrumental tools in saving and starting relationships, marriages and happy lives.
Misconceptions by physicians that implants are bad, and should only be used as a last result treatment. It is funny how my referring physicians have seen how happy my patients are and have come for implants themselves. It is up to us to properly educate the medical communities around us.
Fear of pain is natural and patients worry about this. I reassure them that it is unusual to have extreme pain with implants. I use perioperative penile blocks with long acting anesthetics and give them pain medicine to take home with them. I believe the use of a JP drain can help minimize swelling and hematoma which are by themselves causes of postoperative pain. Patients are reassured that we understand their fear of pain and it is normal, and we will do everything within our power to help them avoid pain.
Some patients can’t get their act together and fail to obtain medical clearance for the surgery. This is where a good surgical coordinator is crucial. The coordinator can all patients and help set appointments for clearance at their medical doctors and arrange for cardiology or other evaluations. The use of Vidscript is interesting for this purpose.
Pre-op and Infection prevention methods:
Patients are given an antimicrobial soap to wash starting 3 days before the surgery and in the morning before they come to surgery. No evidence exists that antimicrobial soap works better than regular soap, but I find patients to be more compliant with showering when you make the soap special. We tell them they can shave at home before coming or we will shave them in the hospital.
All patients are given preoperative antibiotics; we use 1 gram of Vancomycin given over 1 hour and Gentamycin 5 mg/kg before incision. It is imperative that the antibiotics are fully infused before making any incisions as you want high tissue levels of antibiotics.
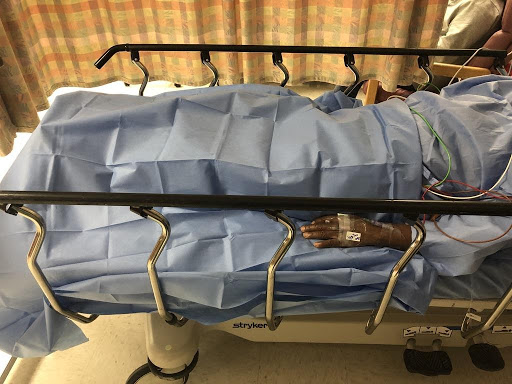
We utilize paper gowns and sheets so as to avoid contamination of the surgical theatre with bacteria in the lint of the bed sheets and gowns.

I do not allow any jackets or blankets within the operating room. In addition to restricting access to the surgical suite by personnel.
Patients are prepped by washing the surgical site with Hibiclens soap, removing it completely and the applying Chloraprep over the surgical field. We apply alcohol to our hand after scrubbing for surgery.

We utilize a very strict no touch technique with frequent glove changes. We use copious amounts of antibiotic irrigation and implant only antibiotic coated implants. We do not insert a Foley catheter for the procedure this prevents the possibility of contamination from the catheter as well as, making the surgery more comfortable to do.
It is important to always change gloves when opening the implant for the very first time. Given all this changes in protocol we have been very successful in almost completely eliminating implant infections.
Fast surgery helps decrease infection rates, you should strive for your implant cases not to last more than 20 minutes’ total surgical time. We will teach you techniques during the course on how to speed up you operating room times.
Unfortunately, infection rates are never zero patients should be aware of this possibility. Doctors that don’t any infected cases either do not operate or lie about it. It is our responsibility as clinicians to constantly evaluate our technique and make changes and adjustments to get the infection rate as close to as zero as possible.
Surgical Technique:
Lateral Scrotal Incision:
I have modified the incision site to sit in the upper lateral part of the scrotum along the Rugae of the scrotum. The incision is placed on the same side of reservoir placement.
Reasons:
1) Incision avoids peno-scrotal junction thereby not having any issues of postoperative pain or scaring at this sensitive part of the penis. I have seen patients with chronic pain following incisions in this area. Also, makes incision invisible once healed.
2) Incision is far away from the Pump of the implant allowing early manipulation of the pump.
3) Most dissection and implant placement is done on that side of the body thereby decreasing post-operative swelling and Hematoma.
Scrotal approach:
- Scar less visible for patients and patient partners
- Better access to entire corpora and improved exposure
- No issues with pump migration
- Penile implant cylinder tubing does not come from above causing less bother for thin patients.

5. My preference
Pearls:
- Use Scott retractor
- Use nasal speculum
- Place table on flex with Trendelenburg, this allows you to get more proximal on the corpora and levels the operating field.

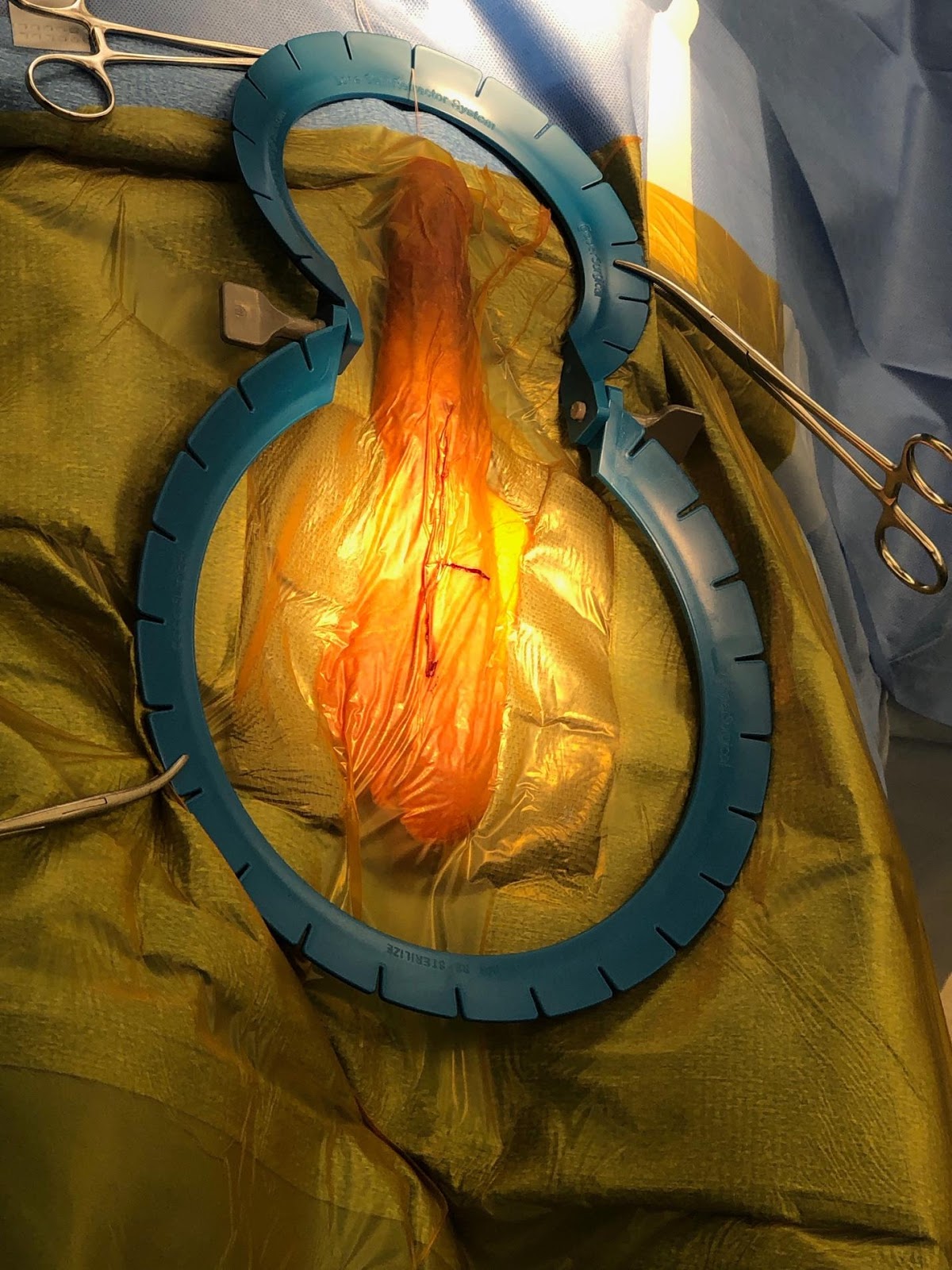
4. Place penis on maximal stretch prior to placement no touch drape, helps dissection and sizing.

5. Place the No touch drape and change gloves
6. Elevate and traction scrotal skin, subcutaneous tissues during the dissection and reposition hooks frequently.
7. Preplace sutures on the corpora prior to opening it. 2-0 Monocryl UR-6 needle. Place them as proximally as possible. Two overlapping stay sutures per side.
8. Do not serial dilate if no fibrosis present, only introduce Furlow.
9. Point Furlow laterally in the direction of the Bone, when passing it proximally to avoid proximal crossover.
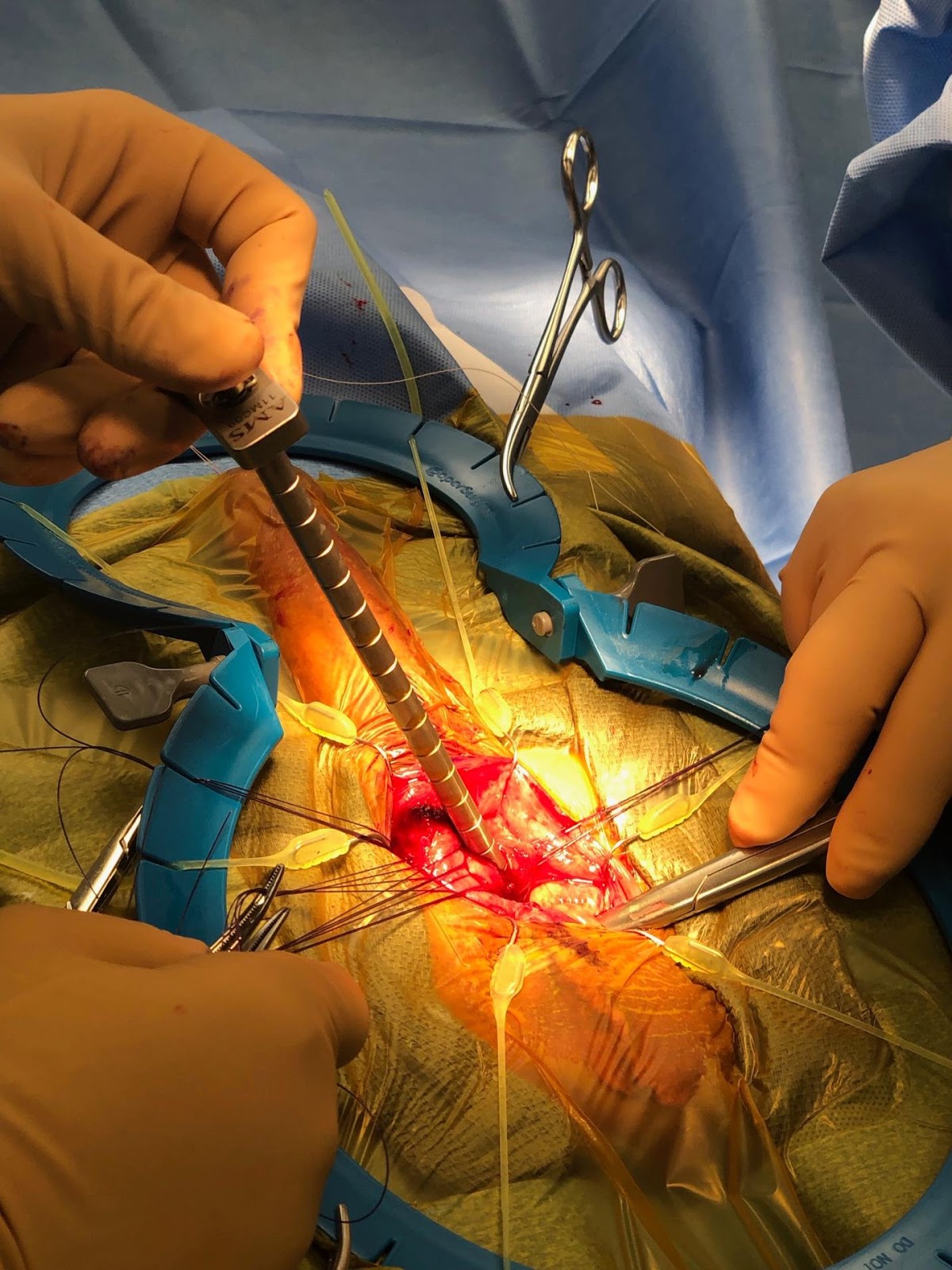
10. Remember surgery is Ballet and not Karate don’t be rough with the Furlow prevent perforations.
11. Stretch penis and close the fossa naviculars with your fingers when passing Furlow distally.
12. Measure proximal and distal measurements as many times as needed to be sure of the cylinder size to use. Avoid rear tips as much as possible.
13. Never pass a Furlow with a needle if the other side cylinder is up the penis. Remove it first.
14. Reservoir placement with finger dissection if possible- Path of least resistance. Don’t be pragmatic.
15. Use curved May scissors and Nasal speculum for pump placement- Dependent portion of the scrotum well away from the testicle.
16. Irrigate, Irrigate, Irrigate
17. Multi layered closure.
18. Do a great job: We need a functional result not a perfect result! Avoid the desire for perfection that leads to maneuvers’ that turn out disastrous.
Postoperative:
1. Ice Packs 20 minutes on 20 minutes off – remember do not put on the skin
2. JP- remove postoperative day number 3
3. Penile implant activation 5-6 weeks
4. Antibiotics for 5 days orally to go home.
Proper pump placement:
Placement of the penile implant pump is one of the most important aspects of the penile implant surgery as this is the part the patient will be accessing the most. The pump for the penile implant has to be placed in the posterior dependent portion of the scrotum. This allows for concealment, ease of operation and does not shorten the effective penile length.
Great Pump Placement:

Bad Pump Placement:


Notice how the pump basically shortens the effective penile length.
Corrected:


Pump moved to a more dependent position which will be totally unnoticeable when healed. Also, notice by removing the pump from the base of the penis the effective useful penile length has been increased.
Pump placement failure occurs:
- When the scrotal dissection for the pump is inadequate
- When the tubing exciting the corpora are too short.
A. Wrong implant size
B. Corporotomies too distal
C. Rear tips not used when needed
D. Infra-pubic implant – pump naturally migrates up and patient not told to manipulate pump early to bring it down.
